Chadwick Boseman’s death has drawn attention to colon and rectal cancer. The 43-year-old actor was diagnosed with stage 3 colon cancer in 2016 and died on Friday. During that time, his family said that he juggled chemotherapy, “countless surgeries” and performances for films ranging from Marshall to Black Panther.
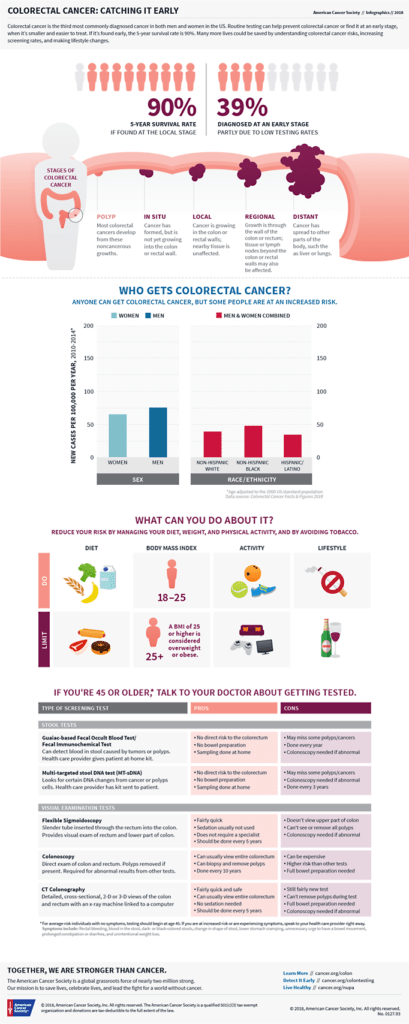
Colorectal cancer is one of the most common forms of cancer. It typically affects people older than 50, but the reasons for the increase among younger people like Boseman are unclear.
“Although the overall death rate has continued to drop, deaths from colorectal cancer among people younger than age 55 have increased 1% per year from 2008 and 2017,” according to the American Cancer Society.
“By the year 2030, colon cancer is estimated to rise 90 percent and rectal cancer to rise by a staggering 124 percent in these young patients,” said Kimmie Ng, MD, MPH, director of the Young-Onset Colorectal Cancer Center at the Dana-Farber/Brigham and Women’s Cancer Center in Boston, said in a statement.
“This highlights the urgency of trying to identify new ways to prevent, treat and catch these cancers earlier at a curable stage.”
That’s partly why the American Cancer Society has reduced its recommended age for colorectal screening from age 50 to 45 for those with average risk.
Having a risk factor is no guarantee that someone will develop colorectal polyps or cancer, but it raises the chances. The good news is that certain risk factors, like diet or smoking, can be controlled.
 Here is information on 13 risk factors for colorectal cancer from the American Cancer Society:
Here is information on 13 risk factors for colorectal cancer from the American Cancer Society:
- Being Black
African Americans have colorectal cancer more often than other racial groups in the United States and the highest death rate, according to ongoing and new research in Statistics and CA: A Cancer Journal for Clinicians.
- Being physically inactive
If you’re not physically active, you have a greater chance of developing colon cancer. Regular moderate to vigorous physical activity can help lower your risk.
- Being overweight or obese
If you are overweight or obese (very overweight), your risk of developing and dying from colorectal cancer is higher. Being overweight raises the risk of colon and rectal cancer in both men and women, but the link seems to be stronger in men. Getting to and staying at a healthy weight may help lower your risk.
- Certain types of diets
A diet that’s high in red meats (such as beef, pork, lamb or liver) and processed meats (like hot dogs and some luncheon meats) raises your colorectal cancer risk.
Cooking meats at very high temperatures (frying, broiling or grilling) creates chemicals that might raise your cancer risk. It’s not clear how much this might increase your colorectal cancer risk.
- Having a low blood level of vitamin D
Following a healthy eating pattern that includes plenty of fruits, vegetables and whole grains, and that limits or avoids red and processed meats and sugary drinks probably lowers risk.
- Smoking
People who have smoked tobacco for a long time are more likely than non-smokers to develop and die from colorectal cancer. Smoking is a well-known cause of lung cancer, but it’s linked to a lot of other cancers, too. Also see: Guide to Quitting Smoking.
- Alcohol use
Colorectal cancer has been linked to moderate to heavy alcohol use. Even light-to-moderate alcohol intake has been associated with some risk. It is best not to drink alcohol. If people do drink alcohol, women should have no more than one drink a day; two drinks a day for men. This could have many health benefits, including a lower risk of many kinds of cancer.
- Having type 2 diabetes
People with type 2 (usually non-insulin dependent) diabetes have an increased risk of colorectal cancer. Both type 2 diabetes and colorectal cancer share some of the same risk factors (such as being overweight and physical inactivity). But even after taking these factors into account, people with type 2 diabetes still have an increased risk. They also tend to have a less favorable outlook after diagnosis.
- A personal history of inflammatory bowel disease
If you have inflammatory bowel disease (IBD), including either ulcerative colitis or Crohn’s disease, your risk of colorectal cancer is increased.
IBD is a condition in which the colon is inflamed over a long period of time. People who have had IBD for many years, especially if untreated, often develop dysplasia. Dysplasia is a term used to describe cells in the lining of the colon or rectum that look abnormal, but are not cancer cells. They can change into cancer over time.
If you have IBD, you may need to start getting screened for colorectal cancer when you are younger and be screened more often.
Inflammatory bowel disease is different from irritable bowel syndrome (IBS), which does not appear to increase your risk for colorectal cancer.
- Night shift work
Some studies suggest working a night shift regularly might raise the risk of rectal cancer. This might be due to changes in levels of melatonin, a hormone that responds to changes in light. More research is needed.
- Having an inherited syndrome
About 5% of people who develop colorectal cancer have inherited gene changes (mutations) that cause family cancer syndromes and can lead to them getting the disease.
- A personal history of colorectal polyps or colorectal cancer
If you have a history of adenomatous polyps (adenomas), you are at increased risk of developing colorectal cancer. This is especially true if the polyps are large, if there are many of them or if any of them show dysplasia. (Adenomatous polyps are the kind of polyps that can become cancer.)
If you’ve had colorectal cancer, even though it was completely removed, you are more likely to develop new cancers in other parts of the colon and rectum. The chances of this happening are greater if you had your first colorectal cancer when you were younger.
If you’ve had adenomatous polyps or colorectal cancer, it’s important to tell your close relatives so that they can pass along that information to their doctors and start screening at the right age.
- A family history of colorectal cancer or adenomatous polyps
Most colorectal cancers are found in people without a family history of colorectal cancer. Still, as many as one in three people who develop colorectal cancer have other family members who have had it.
People with a history of colorectal cancer in a first-degree relative (parent, sibling or child) are at increased risk. The risk is even higher if that relative was diagnosed with cancer when they were younger than 50, or if more than one first-degree relative is affected.
The reasons for the increased risk are not clear in all cases. Cancers can “run in the family” because of inherited genes, shared environmental factors, or some combination of these.
Having family members who have had adenomatous polyps is also linked to a higher risk of colon cancer. If you have a family history of adenomatous polyps or colorectal cancer, talk with your doctor about the possible need to start screening before age 45.