By Robin Fields, ProPublica
British health authorities announced last summer that they’d found evidence suggesting local spread of polio in London.
It was a jolt, to be sure. The country was declared polio-free in 2003.
But at least no one had turned up sick. The proof came from routine tests of sewage samples, which can alert health officials that a virus is circulating and allow them to intervene quickly. Based on genetic analysis of those samples, officials in the United Kingdom moved to protect the city’s children by reaching out to families with kids under 5 who hadn’t been fully vaccinated.
Polio’s first appearance in almost a decade in the U.S., confirmed in July by health officials in New York, would play out quite differently.
In the U.S., public health agencies generally don’t test sewage for polio. Instead, they wait for people to show up sick in doctor’s offices or hospitals — a reactive strategy that can give this stealthy virus more time to circulate silently through the community before it is detected.
In New York, the first sign of trouble surfaced when a young man in Rockland County sought medical treatment for weakness and paralysis in June. By the time tests confirmed he had polio, nearly a month had passed.
Because the majority of polio infections cause no symptoms, by the time there’s a case of paralysis, 100 to 1,000 infections may have occurred, said Dr. Yvonne Maldonado, a professor of pediatrics at the Stanford School of Medicine who chairs the American Academy of Pediatrics’ committee on infectious diseases.
“You’re already chasing your tail if you’re going to wait for a case to show up,” she said.
Only after the case was identified did New York health officials start the sort of surveillance the British did, testing wastewater samples from Rockland County and beyond to help determine if the virus is spreading and where. Like many parts of the U.S., New York already was collecting sewage and analyzing it to track the spread of COVID-19. Health officials say they’re now testing stored samples for signs of polio. They say they’ve detected polio in a few Rockland County samples but need to analyze more to understand what the initial results represent.
For decades, the cost of doing wastewater surveillance for diseases like polio pretty clearly outweighed the benefit.
High U.S. vaccination rates, topping 90%, made the risk of such diseases incredibly low, though there have long been pockets of population in which rates are far lower. Rockland County, a suburban area northwest of New York City, is one such place. It suffered an extended outbreak of measles, another vaccine-preventable disease, in 2018 and 2019 that was largely concentrated in its Orthodox Jewish community, where many opt out of vaccines. Several news organizations have reported that the polio patient is a member of that community.
Nationally and globally, there are signs that the pandemic has opened up new vulnerabilities to diseases long in retreat. Routine immunizations have been hindered by a host of obstacles, including COVID-19-related lockdowns and growing vaccine resistance stoked by misinformation and politicization. A recent analysis by UNICEF and the World Health Organization showed that the percentage of children worldwide who received all three doses of the vaccine against diphtheria, tetanus and pertussis — a measure of overall immunization — dropped 5 points between 2019 and 2021 and that measles and polio vaccinations fell, too. The organizations say that’s the largest sustained decline in childhood vaccinations in the roughly 30 years they’ve been collecting data.
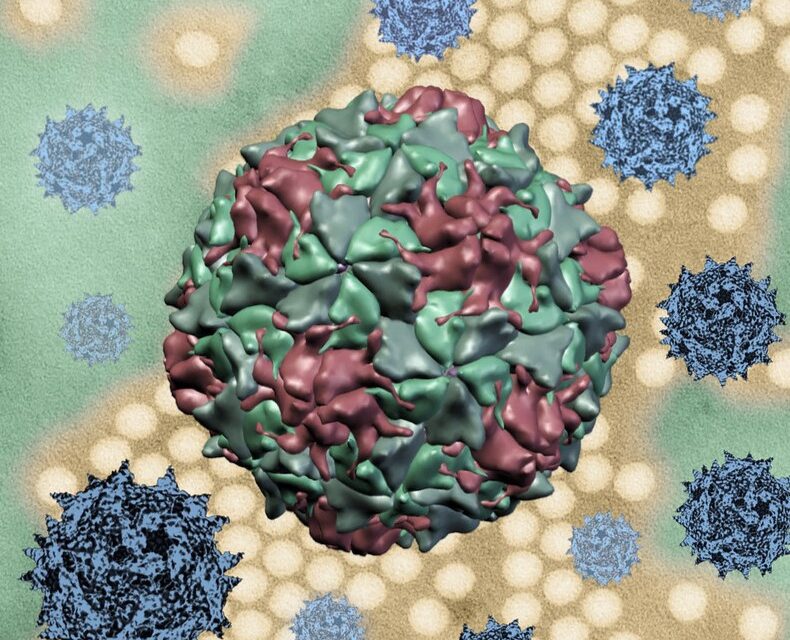
That could create greater risk of polio, a scourge of the first half of the 20th century in the U.S. Highly contagious and potentially life-threatening, polio historically has victimized mostly young children, attacking their spinal cords, brain stems or both.
The virus spreads when fecal material or respiratory droplets from infected people get into water or food or onto other people’s hands, which they then put into their mouths. This may sound unusual, but it’s among the more common ways viruses circulate, especially among children.
Around 70% of those who are infected show no signs of the illness but can infect others. Of those who do get sick, most have mild symptoms, such as fever, sore throat, muscle weakness and nausea. But about 5 in 1,000 infected people develop irreversible paralysis.
At its peak in 1952, polio killed more than 3,000 Americans and paralyzed more than 20,000. Images of children encased in coffin-like iron lungs terrified parents. Those fears faded swiftly after the first polio vaccine was approved in 1955. Within two years, cases dropped by as much as 90%.
Since 1988, when the Global Polio Eradication Initiative began pouring billions into immunization campaigns and surveillance around the world, polio has been eradicated in much of the rest of the world. Wild polio, the kind that occurs naturally, remains endemic in just two countries, Pakistan and Afghanistan.
But there’s another kind of polio that’s circulating, one linked to the type of vaccine that’s used in much of the world, particularly lower-income countries. This oral vaccine, which hasn’t been used in the U.S. since 2000, is easy to administer — just a few drops on the tongue — and cheap to make. It uses weakened live viruses to trigger the immune system to create protective antibodies.
That brings a bonus. When the vaccinated shed the weakened live viruses in their stool, they can spread to the unvaccinated, triggering protective antibodies in them as well.
But it also brings a risk. In rare instances, when the weakened viruses circulate in people who have not had the vaccine or are under-immunized, they revert to a form that can sicken unvaccinated people, causing the disease they were meant to prevent. The injectable polio vaccine used in the U.S. contains only inactivated viruses and cannot cause this.
Cases of vaccine-derived polio have surged in recent years after global health authorities in 2016 decided to remove one strain of polio from the oral vaccine after determining that the wild version had been eradicated globally. That left a growing number of children with no immunity to the vaccine-derived version of that strain, Type 2. (The injectable form of vaccine used in the U.S. conveys protection against all strains of polio.)
Type 2 vaccine-derived poliovirus is the kind that was found in the British sewage samples. It was also the kind that infected the unvaccinated Rockland County man, indicating a transmission chain from someone who received the oral polio vaccine, health officials in New York said.
Officials are still investigating where the man caught the virus, here or abroad. The Washington Post has reported that the man traveled to Poland and Hungary this year, but a spokesperson for the Rockland County Health Department said in an email, “The person did not travel outside the country during what would have been the incubation window.”
Ultimately, New York health officials will use wastewater monitoring to tell them quickly whether they have a bigger problem, essentially allowing them to test thousands of people at once for polio infection rather than individually, David Larsen, an epidemiologist and Syracuse University professor who directs the state’s wastewater surveillance network, said in an email.
Wastewater testing for polio has been a staple in developing nations for decades, but at least a few countries where cases are rare and vaccination rates are high do it, too.
The U.K. began monitoring wastewater in 2016 for polio and several other viruses that occur in the gastrointestinal tract, a spokesperson for the British health security agency said via email. (It has since added the virus that causes COVID-19 to the list.)
Israel has monitored sewage for polio since 1989. In 2013, health officials were able to detect an outbreak of wild polio just from sampling and launch a vaccine campaign in response without ever experiencing a case of paralysis. This year, though, a young child in the Jerusalem area came down with paralytic polio. Public health authorities there found additional infections through sewage tests.
Some U.S. public health officials have been skeptical of the value of such testing here.
“I’ve always been unenthusiastic about doing it for polio in the U.S. and a big supporter of doing it elsewhere, where there are deficiencies in other surveillance systems,” said Mark Pallansch, who retired in 2021 after spending much of his career working on polio eradication efforts for the Centers for Disease Control and Prevention.
COVID-19 has triggered a blast of interest in wastewater surveillance, prompting cities, states and colleges to launch programs and opening a floodgate of funding for them.
The CDC sent federal money to health departments in over 40 jurisdictions to support such tracking efforts, working with them to collect data that’s published on the agency’s National Wastewater Surveillance System website. A spokesperson said in an email that the agency was working to expand the platform to include data on other pathogens, from foodborne infections like salmonella to influenza, but not polio. Testing nationally for polio would be labor and resource intensive, requiring increases in public health laboratory capacity, the spokesperson said.
One asset of wastewater monitoring is the ability to pivot quickly to test something new.
In November 2020, the Sewer Coronavirus Alert Network, based out of Stanford and Emory universities, started daily monitoring at California wastewater plants for the virus that causes COVID-19. It’s since added monitoring for other pathogens, including COVID-19 variants, the common respiratory virus RSV and, most recently, monkeypox. Such additions are relatively economical since the network can test for multiple pathogens from a single sample, said Marlene Wolfe, one of the two principal investigators and an assistant professor at the Rollins School of Public Health at Emory.
In adding more tests, Wolfe said, the question is always whether monitoring a disease this way is likely to surface anything of enough concern to drive public health decisions.
Many question whether the expansion of wastewater testing fueled by the pandemic will last. Maldonado, the American Academy of Pediatrics’ infectious diseases committee chair, said the recent polio case is another signal that more disease tracking is critical.
“Maybe this is a clarion call for us to really start building better surveillance networks,” she said.