With African-American women being more likely to care for elderly family members at home, Todd Shurn is a rarity: a man who became the primary caregiver when his mother, Alice Shurn, was diagnosed with dementia. Older African Americans, especially women, have higher rates of dementia and more complications. This article is Part 1 of an occasional series that will examine such issues along with caregiving.

Alice Shurn with her son, Todd, and goddaughter, Daphne Gibson, at her sorority Delta Sigma Theta’s convention in 2013. (Photos courtesy of Todd Shurn)
By Yanick Rice Lamb
Todd Shurn braces his mother from behind, her arms resting on his as they shuffle into a restaurant in lockstep. Alice Shurn is frail and a fall risk, but she has no chance of hitting the ceramic tile floor. Her only son is determined to keep her safe. It’s what he has done day after day for nearly four years.
It doesn’t matter to Shurn that he’s a single man in a vibrant city like Washington, D.C. When friends try to nudge him out of the three-bedroom house that he shares with his mother for a night on the town, he usually declines. His world orbits around his mother, and he’s OK with that. Their lives are in lockstep.
“My life is dedicated to making her happy,” Shurn says. “The loss of my personal freedom — I’ve accepted that. I can’t do anything.”
Men like Shurn are not as rare as they used to be, but they are still in the minority when it comes to caregiving. Only a third of caregivers are men, according to a study by the National Alliance for Caregiving and AARP. Men are less likely to be the main or only person in this role. They’re less likely to be involved with personal care and more likely to pay for it.
Not Todd Shurn.
He has a sister in Atlanta — more than 700 miles from their family home in Benton Harbor, Mich., and she has two children. So, Shurn does it all with the help of an aide who relieves him when he goes to work at Howard University, where he’s an associate professor in the Department of Systems and Computer Science.
He’s had to learn how to bathe his 83-year-old mother, brush and floss her teeth, feed her, clothe her and comb her hair into something more or less presentable. Today, her silver locks are hidden beneath a gray flapper’s hat with a matching wool flower on the side. Dressed in gray pants with a red-orange sweater over a white turtleneck, she smiles adoringly whenever she glances over at her son next to her in the booth.

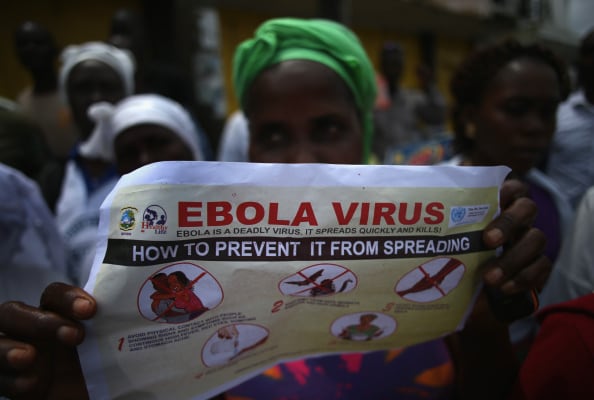
Lewy bodies in the brain. Also see “Understanding Dementia: 5 Top Types” for more information at the end of this article. (Photo: Alzheimer’s Association)
In early 2011, Mrs. Shurn was diagnosed with Lewy body dementia, named for Dr. Frederick H. Lewy who discovered the abnormalities in how the brain processes the alpha-synuclein protein in the early 1900s. Dementia with Lewy bodies (DLB) is the third most common form of dementia after Alzheimer’s disease and vascular dementia. Its brain changes are somewhat similar to those of Alzheimer’s and Parkinson’s disease.
Mrs. Shurn’s brain has a buildup of protein deposits called Lewy bodies in nerve cells that control how she moves, how she thinks and what she remembers. Her shuffled walk, balance problems and hunched posture are classic symptoms. Just before diagnosis, she developed orthostatic hypotension. Her blood pressure would plunge when she stood, causing her to fall — once into the family Christmas tree — or pass out.
The brain cell damage causes fewer memory problems than Alzheimer’s disease, allowing her to reminisce with her son sometimes and maintain her love for piano playing at an adult-care center that she visits on occasion. However, it affects her attentiveness and ability to reason, requiring Shurn to redirect his mother’s hands periodically from sprinkling sugar on the table. He reacts calmly with patience and smooth repetitive motions, like a parent who’s used to moving a child out of harm’s way or minimizing a mess. Every now and then, he says, “Don’t do that,” to no avail.
“It’s sort of like watching childhood development in reverse,” notes R. Scott Turner, M.D., Ph.D., director of the Memory Disorders Program at Georgetown University.